Ever wondered why your gut and mood seem so interconnected? Well, there’s a fascinating world of communication happening between your gut, brain, and the trillions of microorganisms living inside you. Let’s break it down in simpler terms.
How Your Gut Talks to Your Brain
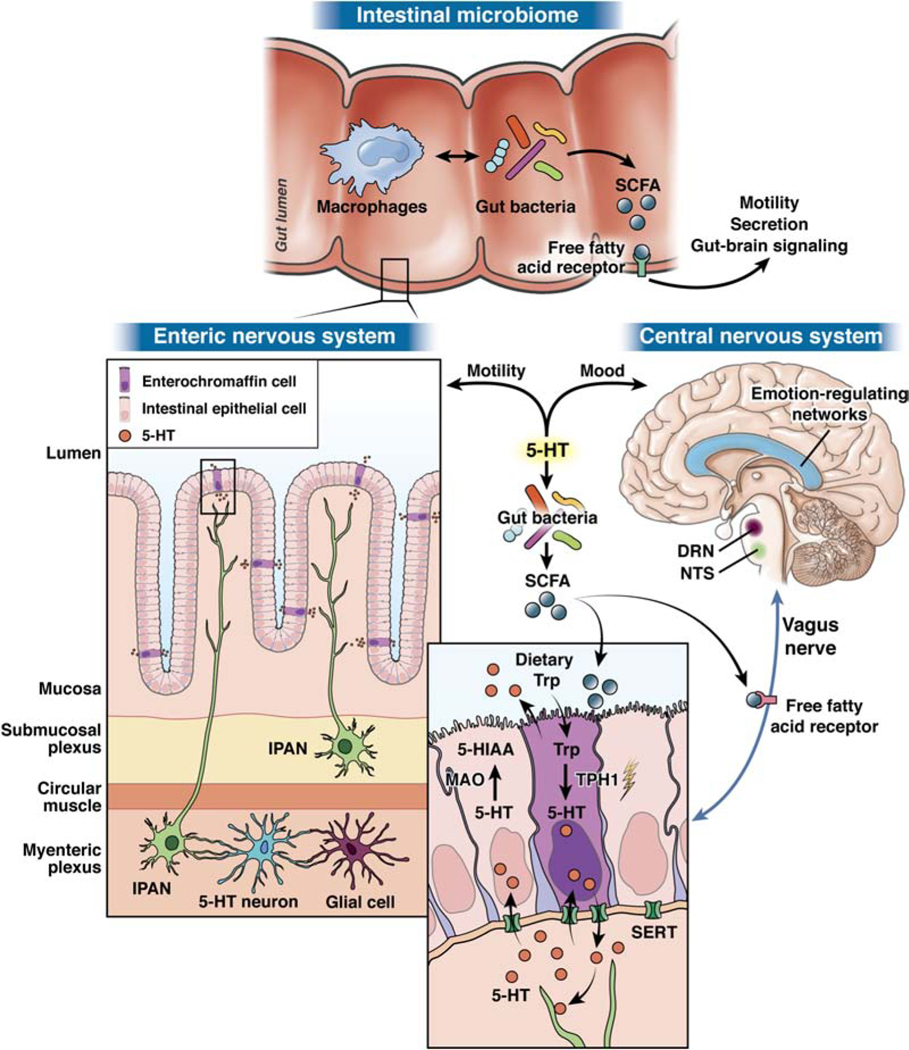
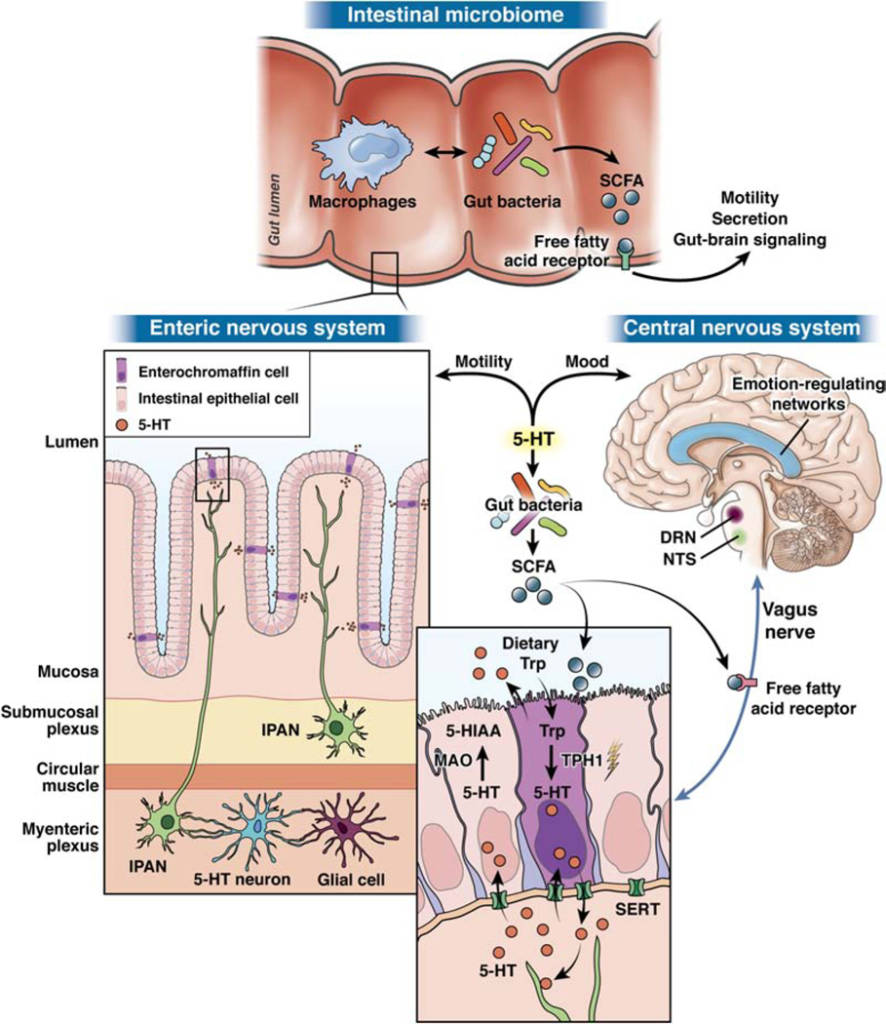
Imagine your body as a complex messaging system where your gut and brain constantly chat. Scientists are uncovering the secrets of this communication network, especially in understanding mood and gut movement disorders. Your gut and brain talk through hormones (like cortisol), immune cells (called cytokines), and nerve pathways. These pathways create bridges between your gut and brain, allowing messages to travel back and forth. Inside your gut, there are tiny microbial superheroes. Some of these microbes can produce special chemicals, like γ-amino butyric acid (GABA), noradrenaline, and dopamine. These chemicals can influence cells in your gut, creating an essential line of communication.
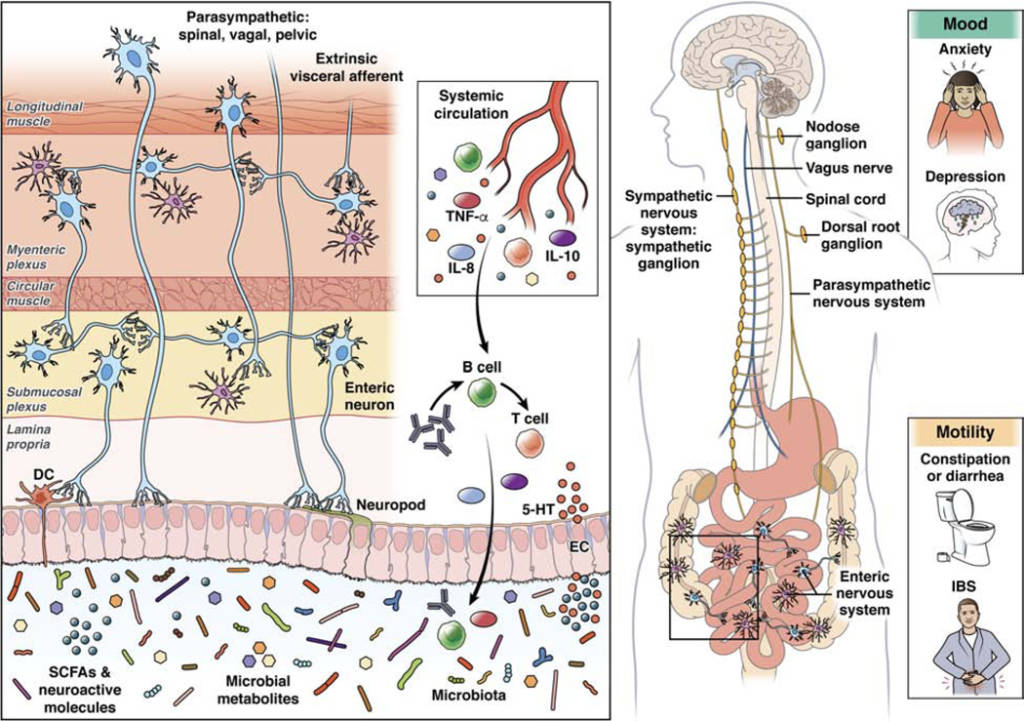
Microbes also create magical compounds that can affect your gut barrier function and immune system. They can interact with different cells, like epithelial cells (the lining of your gut), enteroendocrine cells (EECs, which release hormones), and dendritic cells (important for immune function). Think of these compounds as messengers that can change how your gut and brain work together. Special structures in your gut, like neuropods on EECs and enteric nervous system (ENS) cells, play a crucial role. These structures can send signals to your brain through nerve connections, including the vagus nerve. It’s like your gut has its own messaging system that directly talks to your brain!
However, there’s still a lot to discover about the exact pathways these messages take. Scientists are unravelling this incredible network, opening doors to better understanding and potential treatments for various health conditions.
The Brain-Gut Connection: Ancient Wisdom to Modern Science
Centuries ago, philosophers like Hippocrates hinted at the link between our brain and gut. Fast forward to today, and science has confirmed that our gut and brain are in constant communication. But here’s the twist – your gut’s resident microbes (the microbiota) play a significant role in this chat!
Meet the Microbiota-Gut-Brain Axis: The Ultimate Communicator
Your gut, brain, and microbiota form a complex system known as the Microbiota-Gut-Brain (MGB) Axis. Think of it as a superhighway where signals flow bidirectionally, affecting everything from digestion to mood.
How It Works: A Symphony of Signaling
- Microbial Messages: Your gut microbes talk to your brain through various pathways, including the vagus nerve, neurotransmitters, and bacterial metabolites.
- Gut-Brain Harmony: The gut-brain connection influences your mood, stress levels, and even conditions like Irritable Bowel Syndrome (IBS). Your gut health affects your mental well-being, and vice versa!
The Marvel of Microbial Influence: More Than Just Digestion
Your gut microbiota isn’t just about digestion. It’s linked to the development of your brain, affecting processes like neurogenesis and microglia activation. Even your gut’s motility is influenced by these tiny inhabitants!
Sensitive Stages: From Birth to Adulthood
Early in life, factors like breastfeeding, diet, and stress exposure shape your gut microbiota. These factors impact your gut-brain axis during crucial developmental periods, setting the stage for lifelong well-being.
The Future of Gut-Brain Health: Unraveling the Mysteries
While we’ve made incredible strides, there’s still much to discover. Researchers are exploring the nuances of this intricate relationship, aiming to find new ways to enhance our physical and mental health.
So, next time you trust your gut feeling, know that it’s not just a saying – it’s backed by the fascinating science of the Microbiota-Gut-Brain Axis! Stay tuned for more discoveries that could transform the way we understand and nurture our holistic well-being.
Unlocking the Secrets of the Gut-Brain Connection: How Your Microbiome Influences Your Health
Have you ever wondered why a “gut feeling” is often considered a valid intuition? The connection between your gut and brain is a fascinating and complex interplay of signals that influence not only your digestive system but also your mood and overall well-being. Recent research has shed light on this intricate relationship, revealing the essential role of the microbiota-gut-brain (MGB) axis in maintaining balance within your body.
Understanding the MGB Axis: A Complex Communication Network
The MGB axis refers to the bidirectional communication system between your gut and brain, mediated by the trillions of microbes residing in your digestive tract. These microbes, collectively known as the microbiome, play a pivotal role in modulating the function of both the enteric nervous system (ENS) in the gut and the central nervous system (CNS) in the brain. This intricate network of signals influences various aspects of your health, including digestion, mood, and behaviour.
The Role of Serotonin: A Key Player in the MGB Axis
Serotonin, a neurotransmitter known for its influence on mood regulation, is a central player in the MGB axis. It is produced in abundance in the gut, where it regulates various physiological functions, including motility and secretion. Studies have shown that alterations in enteric mucosal and blood serotonin signalling are observed in individuals with conditions like IBS, indicating a potential link between serotonin dysregulation and gastrointestinal issues.
Picture this: your gut, brain, and the microbes in your gut are all talking to each other! How?
Let me break it down for you.
Inside your gut, there are tiny living organisms called bacteria. These bacteria create something called short-chain fatty acids (SCFAs). SCFAs help in making a special chemical called serotonin (5-HT). Serotonin is like a messenger that carries important signals between your gut and your brain. It’s made in specific cells in your intestines, called enterochromaffin cells (ECC). Once serotonin is made, it travels out of these intestinal cells. It interacts with receptors (think of them as receivers) on nerve cells in your gut. These nerve cells are part of what we call the enteric nervous system. Serotonin helps control how your gut moves, and during your growth, it even helps your brain cells develop and differentiate.
But the serotonin story doesn’t stop there! Some nerve signals travel from your gut to specific parts of your brain – the nucleus of the solitary tract (NTS) and the dorsal raphe nucleus (DRN). These brain areas are home to most of your brain’s serotonin neurons.
These brain areas then connect with networks that control your emotions and mood. So, the serotonin made in your gut can influence how you feel!
Apart from the serotonin path, SCFAs can also directly interact with receptors in various cells, including nerve cells like the vagus nerve. This interaction affects how your gut moves, the chemicals it produces, and how it communicates with your brain.
In short, serotonin acts as a crucial messenger between your gut, brain, and the microbes in your gut. It’s a fascinating way your body keeps everything in balance!
Microbial Metabolites: The Significance of Short Chain Fatty Acids (SCFAs)
The gut microbiota produces metabolites, such as Short Chain Fatty Acids (SCFAs), that regulate gut-brain signalling. SCFAs like acetate, propionate, and butyrate influence the morphology of microglia in the brain and can reverse the effects of chronic stress. These microbial metabolites also have the potential to impact the production of neurotransmitters in the brain, although further research is needed to understand their precise mechanisms of action.
Immune Mechanisms and Gut-Brain Signaling
An intact immune system is crucial for maintaining a delicate balance between tolerating beneficial gut microbes and defending against harmful pathogens. Toll-like receptors (TLRs) and other components of the immune system mediate the response to microbes and play a role in gut-brain signalling. Dysregulation of these immune mechanisms can lead to conditions like IBS and neurodegenerative disorders, emphasizing the importance of a well-functioning immune system in maintaining overall health.
Disorders of the MGB Axis: IBS and Depression
Disorders of the MGB axis, such as IBS and depression, have significant brain and gut components. Individuals with IBS often experience alterations in gut microbial composition, although the exact role of dysbiosis in symptom development remains unclear. Similarly, patients with Major Depressive Disorder (MDD) exhibit altered gut microbiome composition, raising the possibility of a causal relationship between the microbiota and mental health conditions.
Exploring Therapeutic Interventions: Probiotics, Diet, and Fecal Microbiota Transplantation
Researchers have explored various interventions to target the MGB axis, including probiotics, dietary modifications, and faecal microbiota transplantation (FMT). While probiotics, including strains of Bifidobacterium and/or Lactobacillus, have shown promise in improving symptoms of IBS, more research is needed to establish their efficacy. Dietary approaches, such as the low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) diet, have been effective in managing IBS symptoms in the short term. FMT studies are ongoing, and their outcomes may provide valuable insights into the potential therapeutic role of gut microbiota manipulation.
Challenges and Future Directions: Unraveling the Complexity of the MGB Axis
Despite significant progress in understanding the MGB axis, several challenges remain. The influence of factors like sex and race on microbial diversity and its relationship with brain-gut disorders requires further exploration. Additionally, translating preclinical findings into effective therapies for human brain disorders is a complex task, necessitating a comprehensive understanding of the microbiome-gut-brain interactions.
In conclusion, the MGB axis represents a groundbreaking area of research that holds the key to unravelling the mysteries of the gut-brain connection. As scientists delve deeper into this complex network, new diagnostic methods and therapeutic approaches may emerge, offering hope for individuals affected by disorders of the MGB axis. While the field is still in its infancy, the potential impact on mental and gastrointestinal health is profound, paving the way for innovative solutions and a deeper understanding of the intricate relationship between the gut and brain.
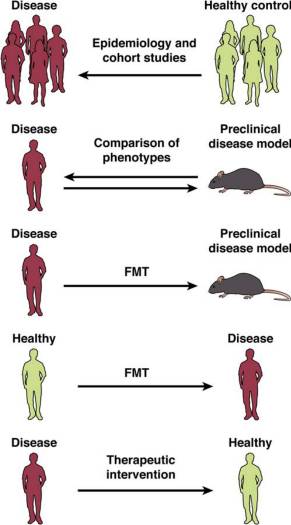
Challenges in Translational Research Explained with a Simple Image
Imagine a puzzle with different pieces that scientists are trying to put together. These pieces represent different ways of studying the connection between the gut microbiome and brain disorders in humans.
Researchers have looked at the bacteria in the guts of people with specific brain disorders and compared them to those without these issues. They’ve found differences in the types of bacteria in these two groups.
Scientists have created special mice that mimic human brain diseases. By studying these mice, they’ve learned more about how these diseases work in our brains.
Researchers have taken bacteria from people with brain disorders and put them into mice without any bacteria. This changed how the mice behaved, similar to the symptoms seen in humans. When they tried the same method with humans, using healthy bacteria in people with brain issues, the results weren’t as clear. It didn’t consistently improve their symptoms.
So far, treatments specifically targeting the microbiome haven’t been very effective. Scientists are still working hard to find ways to help people with brain-gut disorders.
In simple terms, researchers are like detectives, trying to understand the relationship between our gut and brain. They’ve made progress, but there’s still a lot to uncover.
Reference: The Microbiota-Gut-Brain Axis: From Motility to Mood